In this article, we look at the sources and pathways of endocrine-disrupting chemicals (EDCs) entering our bodies, the bioaccessibility–bioavailability–bioactivity continuum of EDCs, and how they may be associated with human allergies.
Endocrine-disrupting chemicals
EDCs are chemicals that can interfere with hormone-signalling pathways in the body. They are ubiquitous in the environment and can cause reproductive abnormalities, neurological defects, allergies and cancer. There is increasing evidence that EDCs contribute to the development of allergic diseases, or allergies. These are clinical conditions caused by hypersensitivity of the immune system to generally harmless foreign proteins and substances.
Humans are exposed to EDCs through food, personal care products, cosmetics, pharmaceuticals, pesticides, plastics, water and soil. The most common EDCs include brominated flame retardants such as per- and poly-fluoroalkyl substances (PFAS), halogenated aromatic compounds such as polychlorinated biphenyls, plasticisers such as dibutyl phthalate, and pesticides such as chlorpyrifos and atrazine. Cadmium is also considered to be an EDC because there is evidence that it harms the reproductive system. Although most EDCs are synthesised, they also exist naturally. For example, soy-based products are a rich source of naturally occurring phytoestrogens.
The bioaccessibility–bioavailability–bioactivity continuum
The toxicity of ingested contaminants – including EDCs – is determined by the bioaccessibility–bioavailability–bioactivity continuum (Figure 1), which is:
- the extent to which they are solubilised in the gut (bioaccessibility)
- their permeability to, and subsequent circulation in, the blood (bioavailability)
- their assimilation and metabolic action in any tissues that subsequently absorb them (bioactivity).
Bioaccessibility is usually evaluated in vitro by physiologically based extraction tests and gastrointestinal digestion procedures. Bioavailability, which expresses the fraction of the bioaccessible compound that enters the blood circulation, refers to the rate and extent to which the compound permeates through the intestinal epithelial cells. Bioactivity refers to the physiological and metabolic interactions between the compound and the human tissue or organ, which disturb homeostasis (the body’s usual healthy equilibrium). EDC toxicity can be mitigated by reducing the permeability in the intestine, thereby reducing the amount of EDC entering the systemic circulation.
EDCs and the allergy link
Our team, in collaboration with Professor Yong Ok (Korea University), is examining the bioaccessibility–bioavailability–bioactivity continuum of EDCs, and their capacity to induce allergic disease.
EDCs interfere with hormone biosynthesis and metabolism, thereby altering normal homeostatic control or reproductive function. Animal models, human clinical observations and epidemiological studies implicate EDCs as a significant contributor to male and female reproductive abnormalities. Hormones such as oestrogen promote the release of histamine, which is responsible for such allergy symptoms as watery eyes, coughing and nasal congestion. If a person ingests EDCs that subsequently interfere with the synthesis and circulation of oestrogen, this can increase the allergic response. The hormone–allergy connection is further supported by the relationship between progesterone and cortisol. Cortisol, a natural anti-inflammatory hormone, is produced in the adrenal glands from progesterone. Any EDC-induced disturbance to, or imbalance in, this hormone system can trigger allergies.
Exposure to EDCs alone may not lead to allergies; however, co-exposure of EDCs with known allergens (eg ovalbumin from egg whites) can enhance the hypersensitivity response to that allergen. When a person is exposed to an allergen for the first time, the body becomes sensitised and produces antibodies against the foreign proteins as an immune response. When exposed to the allergen again, the immune system produces large numbers of antibodies that lead to activation of mast cells containing histamine, thereby causing allergy symptoms. Regular exposure to EDCs in food contaminants amplifies this allergic sensitisation through a form of oxidative stress (an imbalance in the body’s ability to use antioxidants to counteract the harmful effects of free radicals) that promotes the development of allergic symptoms. Thus, EDC exposure may augment the allergic responses to other environmental allergens.
The cause of food allergy is unknown, although dietary chemicals have been suggested to play a role in sensitising our immune system. Our research linking EDCs to allergy will help us to understand some of the physiological and molecular mechanisms for EDC-triggered allergy symptoms. This work will inform future research that will help researchers and clinicians explore new avenues, methodologies and approaches to the mitigation and treatment of EDC-induced allergic diseases, eventually leading to improved clinical treatment and desensitisation of allergies.
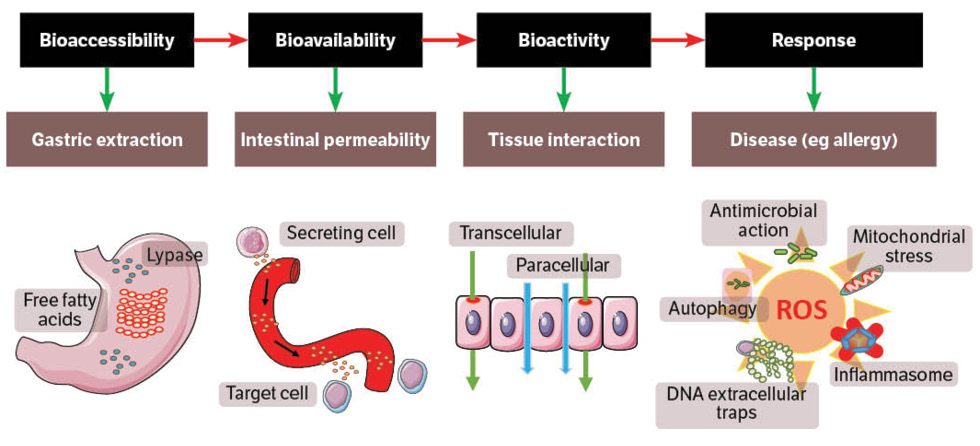
ROS = reactive oxygen species