The global population is 7.2 billion and growing. Around the world, nearly 250 babies are born every minute. This equates to 131.4 million births per year. Despite this global ‘baby boom’, the total fertility rate (TFR) – the number of babies born per woman – has declined by about half over the past 5 decades.
Infertility could be contributing to the drop in TFR. Approximately 15% of couples are infertile, and male infertility contributes to half of the cases. Semen quality has been declining over the past decades, consistent with the drop in TFR. In 1940, the sperm concentration was 100 million counts/millilitre, which dropped to 60 million counts/millilitre in 1990.1 The percentage of motile sperm also declined by about 0.6% per year from 1973 to 1992.2
Male infertility can be influenced by several factors, including genetic, occupational and lifestyle, and environmental. This article focuses on the environmental factors.
The research in this article is part of CRC CARE’s Cleaning Up research program, which develops technologies and strategies for in situ contaminated site remediation.
How are we exposed to environmental pollutants?
Nearly all the commercial products in our everyday life contain different toxic chemicals, which can enter the air, soil and groundwater. Humans can be exposed to these chemicals by either using them or being exposed to them through the environment, and during all life stages – as adults, children and even during pregnancy (in utero).
After exposure, some pollutants may end up in the circulatory system, which can carry chemicals to distal organs and cross physiological barriers of the body (such as the blood–brain barrier and the blood–testis barrier), and accumulate in organs. Toxicant accumulation in the male reproductive organs could risk the normal function of male germ cells – spermatozoa.
How can environmental pollutants disrupt normal cellular functioning?
The following environmental pollutants are considered to be reproductive toxicants:
- polychlorinated bisphenyls
- perfluorinated alkyl substances
- parabens
- phthalate esters
- heavy metals – lead, cadmium, arsenic and uranium
- polycyclic aromatic hydrocarbons
- nanoparticles
- pesticides.
Environmental pollutants can negatively affect the male reproductive function by generating reactive oxygen species (ROS) and causing oxidative stress. ROS and oxidative stress both damage cells. The pollutants may also disrupt the anti-oxidative capacity of organisms. Anti-oxidative enzymes protect cells from the harmful effects of oxidative stress. In human sperm, oxidative stress and disruption of anti-oxidative enzymes may lead to poor sperm motility, low sperm count and sperm DNA damage, all of which compromise fertility.
Men are exposed to these environmental pollutants every day, which may result in declining sperm quality. Some of these toxicants have been detected in blood, urine and semen. Several studies have shown increased levels of these chemicals in infertile men compared with fertile groups, suggesting that these toxicants play a role in infertility.
What do we know so far?
Animal models have provided evidence that some environmental pollutants can compromise production and maturation of spermatozoa (spermatogenesis), and impair sperm function. Although there are clear correlations with certain pollutants, there is not enough information available to correlate exposure to some of the emerging environmental toxicants with male fertility. To properly understand the environmental causes of infertility, we need to broaden our knowledge of how some toxicants affect semen quality.
Parabens as possible culprits
Parabens are alkyl esters of p-hydroxy benzoic acids, and are widely used in cosmetics, pharmaceuticals and foods. The most commonly used parabens are methyl, ethyl, propyl and butyl esters, and are mixed in consumer products as preservatives (together, these parbens have antimicrobial properties). Therefore, people are likely to be exposed to several parabens from the same source at the same time. Parabens act as endocrine disruptors and disturb sperm function in laboratory mice.
Our group recently showed that a mixture of parabens was acutely toxic to human sperm. We exposed human sperm to a paraben solution containing equimolar concentrations of methyl, ethyl, propyl and butyl parabens for 24 hours. Sperm motility and vitality started to drop at a total of 1 mM paraben concentration (that is, 250 µM of each paraben). Cellular superoxide anion (cytosolic ROS) percentage and caspase activity were used as oxidative stress markers. Both markers were increased, meaning ROS was induced in a dose-dependent manner (Figure 1).
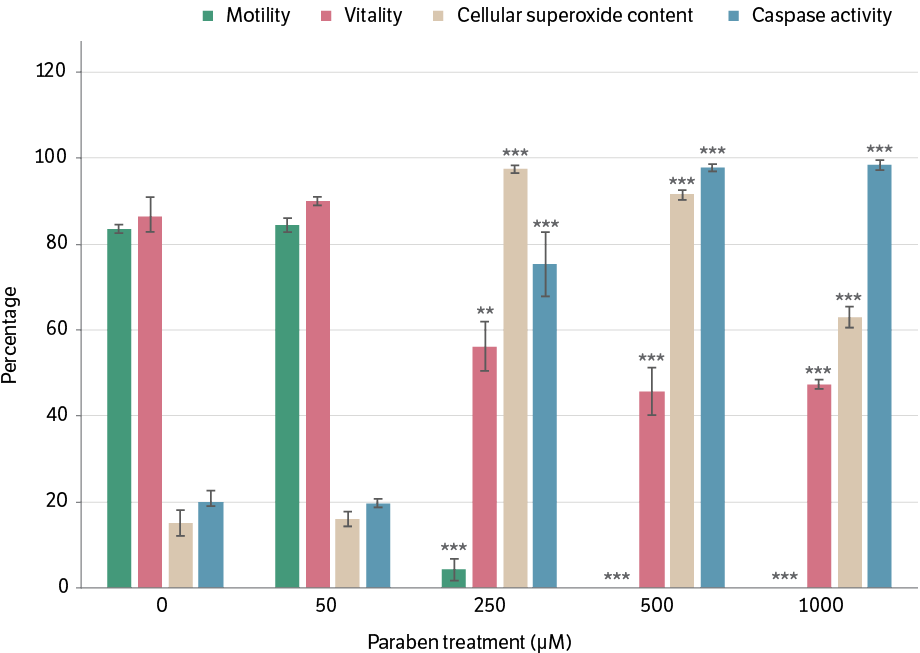
**P < 0.01; ***P < 0.001
Notes: Treatment concentration shown in the graph indicates the concentration of each paraben in the equimolar mixture. Motility, vitality, cellular superoxide content and caspase activity are markers of sperm function and oxidative stress.
What do the results mean?
This study reveals that human sperm function is negatively affected by an acute exposure to a 1 mM mixture of parabens. However, the general population is unlikely to be exposed to a such high concentrations of parabens through the environment. It is possible that chronic exposure to low levels would result in long-term negative effects. Also, multiple toxic chemicals in the environment may be harmful on their own or in combination with each other.
Studying the potential risk of environmental pollutants on sperm quality is important for public health, because these toxicants are so common in the environment. Expanding our knowledge about the effects of toxicants will help to:3
- initiate and amend regulatory requirements (eg listing substances that affect semen quality)
- establish and identify likely exposure places, which would
- make it easier for pregnant women to avoid environmental exposures during pregnancy
- identify and prioritise remediation technologies for high-risk environments
- manage the harmful effects (eg guidance for couples about anti-oxidant therapies).
More epidemiological and reproductive toxicity studies are needed, to assess risk and start public health initiatives.

Human sperm under a microsope
References
- Irvine S, Cawood E, Richardson D, MacDonald E, Aitken J (1996). Evidence of deteriorating semen quality in the United Kingdom: birth cohort study in 577 men in Scotland over 11 years. BMJ 312(7029):467–471.
- Auger J, Kunstmann JM, Czyglik F, Jouannet P (1995). Decline in semen quality among fertile men in Paris during the past 20 years. NEJM 332(5):281–285.
- Mortimer D, Barratt CL, Björndahl L, De Jager C, Jequier AM, Muller CH (2013). What should it take to describe a substance or product as ‘sperm-safe’. Human Reproduction Update19(Suppl. 1):i1–i45.